To view this content, you must be a member of Coding's Patreon at $1.00 or more
Already a qualifying Patreon member? Refresh to access this content.
A question I commonly answer is whether it is okay to report more than 1 unit of a particular CPT code. This is a very valid question when you are looking at a report that describes multiple procedures that would be reported with the same CPT code. A great resource to help with these questions is the Maximum Unit Edits (MUEs) that are published by Medicare each quarter. While this resource is payer specific (meaning it is Medicare’s rules for how many units of a code they would consider appropriate and payable), many mainstream commercial payers like United Healthcare follow Medicare’s payment policies. So starting here can give you great insight on whether you have a good understanding of the code and the guidelines to appropriately use the code. If you find yourself routinely coding in excess of the MUE for a code, it is a signal to pause and review the guidelines and the code definition because it would be unlikely that coding in excess of the MUEs on a routine basis is correct.

You can find the Maximum Unit Edits for Medicare at the following link: CMS MUEs. These edits are updated every quarter so when you arrive at the website, scroll down to the “Downloads” box at the bottom of the page and click on the link for the latest edit file (at the time of publication of this article, this would be the Practitioner Services MUE Table – Effective -10-01-2020 when coding professional services for physicians and other qualified healthcare providers):
Once you click on the link, you will be offered an option to open or save the file. I would encourage you to save the file to your computer for easy access. Be sure to go back to the website and download a copy of the current edit file each quarter.
Once you have your file downloaded, you will want to get familiar with the format of the file and the information it can provide:
Let’s work through a couple of examples to see how the MUE tables can help you code with accuracy.
Example #1: Is it appropriate to code more than one unit for suture of the brachial plexus (CPT 64861)?
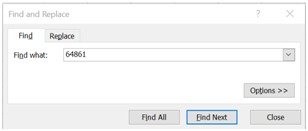
Answer Example #1: With the MUE file open on your computer, hit the Ctrl and F keys on your keyboard to bring up a search box. Type in 64861 and hit enter to search for the CPT code:
You should now see the search results below:
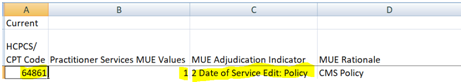
We can see that CPT 64861 has an MUE of 1 unit in column B and the MAI in column C is “2: Date of Service Edit” with a rationale of “CMS Policy” in Column D. This means that you may only report 1 unit of the code when submitting a claim to Medicare or a payer following their payment policies. With the MAI of 2: Date of Service, it would be considered a coding error to report more than 1 unit of the code.
Example #2: How many units of CPT 92920 (angioplasty single major coronary artery or branch) may be reported during the same encounter?
Answer Example #2: With the MUE file open, search for 92920 following the steps described above in example #1. You should now see the following search results:
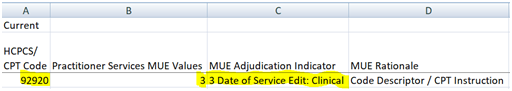
We can see that CPT 92920 has an MUE of 3 units in column B and the MAI in column C is “3: Date of Service Edit” with a rationale of “Code Descriptor/CPT Instruction.” So we could report up to 3 units of 92920 during a single encounter without receiving a denial. We could also report more than 3 units in the rare case that documentation supported doing so. Before submitting the claim, though, we need to first consult the CPT code description and the CPT instructions for use of the code to make sure we are coding appropriately. To illustrate this, a CPT guideline that is critical for coding interventions like angioplasty in coronary arteries is that “Only one base code from this family may be reported for revascularization of a major coronary artery and its recognized branches.” The guidelines also define the major coronary arteries and their recognized branches: “Major coronary arteries: The major coronary arteries are the left main, left anterior descending, left circumflex, right, and ramus intermedius arteries. Coronary artery branches: Up to two coronary artery branches of the left anterior descending (diagonals), left circumflex (marginals), and right (posterior descending, posterolaterals) coronary arteries are recognized.” Considering all of these guidelines, you cannot code more than one base code like 92920 in a single major coronary artery with its associated branches which means it is only possible to report up to 5 base codes in any one case (based on the number of recognized major coronary arteries). The MUE of 3 is set for CPT 92920 because it is highly unlikely to report more than 3 angioplasties in these 5 recognized major coronary arteries/families during the same encounter. So while the MAI would allow you to code in excess of the 3 units, you should pause and carefully review guidelines and documentation to make sure you are doing so correctly before coding in excess of those 3 units.
I hope that helps to illustrate use of this invaluable tool to assist with accurate coding.
Can you code a hernia repair in addition to another abdominal procedure performed during the same surgery? It depends on the relationship between the site of the hernia and the incision for that abdominal procedure.
Valuable guidance on this topic can be found in the NCCI Policy Manual, Chapter 6, section E.4, which states: “If a hernia repair is performed at the site of an incision for an open or laparoscopic abdominal procedure, the hernia repair (e.g., CPT codes 49560-49566, 49652-49657) is not separately reportable.
The hernia repair is separately reportable if it is performed at a site other than the incision and is medically reasonable and necessary.”
As you can see, we first need to identify if the hernia repair occurs along the incision line for another abdominal procedure. Note that this incision could be a large open incision such as a midline incision or it could be a smaller incision to place a port for a laparoscopic procedure. Either way, if the hernia is along the incision site, you cannot report the repair separately. Why? The revenue associated with every CPT code for an open or laparoscopic abdominal procedure already gives the surgeon credit for opening and closing the abdomen. This makes sense because you cannot perform an open or laparoscopic procedure of the abdomen without making some kind of incision in the abdominal wall and then repairing that incision. A hernia is a defect in the wall of a body cavity that allows the organs to protrude from their normal location. In the case of hernias along the abdominal wall, you have a defect (or an abnormal opening) in the layers of the abdominal wall. The surgeon is already being paid to make an incision through the layers of the abdominal wall to reach the abdominal cavity and the organ(s) requiring surgery. So if there is a defect there already, and the surgeon makes an incision through that defect, part of the abdominal wall was already open for him. When closing, the surgeon then has to suture or staple all the layers of the abdominal wall. In doing so, he will incidentally repair any hernia defect in the layers of the abdominal wall along that incision. For this reason, hernia repairs at the site of incisions for another abdominal procedure become part of opening and closing the abdomen. Since the surgeon is already paid to open and close the abdomen when reporting the CPT for the other intra-abdominal procedure he just performed, reporting the hernia code for a repair in that same location would be “double dipping” and reporting the same work twice.
You can report a hernia repair code and a code for an intra-abdominal procedure together if the hernia is repaired at a separate site through a separate incision from the open or laparoscopic incisions used for the intra-abdominal procedure. In this case, there is no “double dipping” on the opening and closing of the abdominal wall because the intra-abdominal procedure requires an incision into the abdomen and repair of the abdominal wall, and the hernia at a separate site also requires an incision into and repair of the abdominal wall so there is distinct work being performed. The hernia repair must be medically necessary and not incidental as well per this guideline – ensuring there is medical necessity is a given for any procedure we code, though.
Finally, you may notice that there are specific ranges of CPT codes listed in this guideline from the NCCI Policy Manual (49560-49566 and 49652-49657). Many coders assume that because there are specific code ranges listed that the guidelines only apply to hernia repairs that would be reported with these codes. However, the code ranges are preceded by an “e.g.” which means “for example.” So this guideline is not restricted only to ventral/incisional hernias. It might also apply to an umbilical hernia, epigastric hernia, or other more specific hernia repairs that are reported with different CPT codes when those repairs occur along an incision for another intra-abdominal procedure. These hernia repairs would be bundled when performed along the incision line for open or laparoscopic abdominal procedures for the same reasons explained above.
Sources: NCCI Policy Manual for Medicare Services – Effective January 1, 2020: https://www.cms.gov/Medicare/Coding/NationalCorrectCodInitEd